Community health workers are crucial to pandemic response. How to support them
The World Health Organisation (WHO) recommends that each country should have a minimum of 445 healthcare workers – such as doctors, nurses, and midwives – for every 100,000 people. But in sub-Saharan Africa, the ratio of healthcare workers to the population is very low: 46 out of 47 countries have significantly less than this figure, though it does vary. For instance, in Rwanda there are 10 doctors for every 100,000 people, while in Kenya there are 20 and in Botswana there are 40.
Since the 1970s, African countries have used community health workers to address gaps in the health workforce. These are local volunteers trained to provide basic health services.
They have effectively supported efforts to manage pandemics, including malaria, pneumonia and diarrhoea, HIV and Ebola. Their role is important because they can be trained to recognise symptoms, diagnose certain diseases, and even dispense medication. In addition, because they are long-time residents in their communities, they are known and trusted sources of information.
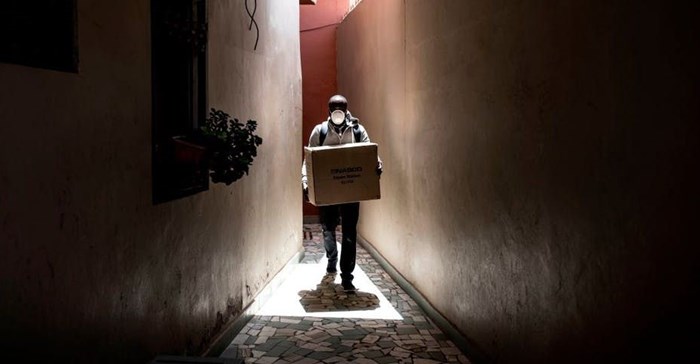
To help deal with the Covid-19 pandemic, some countries like Kenya and South Africa have already mobilised community health workers. In Liberia they are helping to implement prevention and control measures.
But community health workers still face many challenges. For instance, they’re often not compensated enough for the work they do and aren’t given proper direction or training.
It’s important that these challenges are addressed so that they can be more effective – and better supported – when they carry out their work.
Challenges
The WHO has established a number of criteria for effective community health programmes in the Covid-19 response. The advice is to include them – at all levels – in emergency response forums, equip them with essential knowledge and skills, clarify their roles and responsibilities, and provide them with essential tools to protect themselves from Covid-19 and prevent the spread of the virus.
But previous research shows that these boxes may not always be ticked.
A study into the effectiveness of community health workers during the 2014-2016 West Africa Ebola outbreak found that the maintenance of primary care services and the Ebola response were hampered because community members were engaged late in the response.
A reason for this is that community health workers are poorly integrated into existing health systems. Countries didn’t build the management and training structure required for effective integration. A study in South Africa on the governance of community health worker programmes showed that this creates fragmentation in health care delivery and means the community health workers don’t contribute to important decisions.
Compensation
Another big concern is that community health workers don’t get enough support or aren’t well protected. Many, but not all, community health workers work as volunteers and therefore receive no, or very little, monetary compensation.
This was highlighted in the Ebola study. In the three Ebola-affected countries they received very small travel allowances. Without compensation workers couldn’t always make themselves available for their voluntary activities because of other commitments that brought them an income. It also meant that they couldn’t be held accountable for their responsibilities because they weren’t being paid.
This is a common challenge. A recent study on HIV service delivery in low-income countries found that, even though community health workers conduct emotionally and physically demanding tasks, their costs aren’t covered. For instance, they would have to pay their own transport fees to perform a job. This has an impact on the care they can provide and can also lead to them feeling disempowered.
The study also found that they often don’t have adequate training and supervision. Many community health workers have had their responsibilities poorly explained to them, causing some to assume roles that otherwise belong to higher paid and trained staff. This raises an issue of injustice and unfairness in management and treatment of community health workers and jeopardises the future of their profession.
A lack of support and supervision can also be found elsewhere. A study in Kenya saw that in some cases, community health workers are spoken about or spoken for, but receive little support in practice.
Moving forward
Moving forward, governments must ensure that there is better coordination, political commitment and investment when it comes to community health workers.
Authorities should consider setting a minimum standard of compensation and community health workers and local authorities should openly talk about the burdens that workers may face and the need for solutions to overcome them. For instance, if community health workers have to travel long distances, resources such as bicycles should be set into programme budgets.
Community health workers should also be given more say in how programmes are designed. This will tap into their experience and make the aims more achievable in practice.
This article is republished from The Conversation under a Creative Commons license. Read the original article.![]()
Source: The Conversation Africa

The Conversation Africa is an independent source of news and views from the academic and research community. Its aim is to promote better understanding of current affairs and complex issues, and allow for a better quality of public discourse and conversation.
Go to: https://theconversation.com/africa


































