
Top stories






LifestyleWhen to stop Googling and call the vet: Expert advice on pet allergies from dotsure.co.za
dotsure.co.za 2 days
More news
















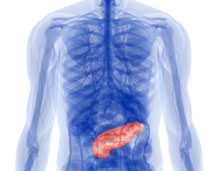
Until now there has been no effective method for imaging pancreatic islet beta-cell mass in a non-invasive manner. Based on the work of Paul Harris and colleagues at Columbia University, the Yale team focused on the genetically expressed protein known as vesicular monoamine transporter type 2 (VMAT2). This protein facilitates the storage and release of some neurotransmitters, and is expressed simultaneously with insulin in pancreatic beta cells.
The Yale team infused both healthy patients and those with type-1 diabetes with a radioactive tracer that targets VMAT2. Patients were then scanned with a PET camera to calculate the radioactivity concentration in the pancreatic cells and measure the binding of the tracer.
Adjusting for dosage and body weight, the radiotracer binding among pancreatic cells was 40 percent less in type-1 diabetes patients than in healthy patients.
Senior author Gary W. Cline, associate professor of endocrinology at Yale School of Medicine, explained, "This tells us that we can now measure the loss of the pancreatic islet cells that produce insulin in diabetic patients. Being able to make these measurements will help in the development of a drug that can stop or slow the death of these cells, and thus prevent the damaging effects of type 1 diabetes."
Other authors are Marc D. Normandin, Kitt F. Petersen, Kevin C. Herold, Yu-Shin Ding, Shu-Fei Lin, Sarita Naik, Krista Fowles, and Richard E. Carson of Yale; Daniel M. Skovronsky of Avid Radiopharmaceuticals; and Timothy J. McCarthy, Judith L. Treadwell, and Roberto A. Calle of Pfizer Global R&D.
This study was funded by the Yale-Pfizer Bioimaging Research Alliance, grants from the National Institutes of Health, the Yale Clinical and Translational Science Award from the NIH, and a Distinguished Clinical Scientist Award from the American Diabetes Association.