Prostate cancer is often missed or under graded using standard biopsy techniques, once again highlighting the low priority of men's health concerns on the agenda.
A biopsy, the most reliable method of detection, is a challenge because of the difficulties in visualising potentially cancerous areas of the prostate, but also the location of the biopsy needle. Trans-rectal ultrasound-guided prostate biopsy (TRUS), the current biopsy standard, can be compared to looking for a needle in a haystack, with poor image resolution; the biopsy needle often passes through tumour-free areas of the prostate – potentially missing the tumour entirely.
“Current detection methods – namely prostate-specific antigen (PSA) tests and digital rectal exams (DRE) – lack specificity and are often inconclusive leading to many uncertainties for both patient and urologist,” says Dr Greg Boustead, specialist urologist and robotic surgeon at Netcare Waterfall City.
“A lack of clear imaging has led to substantial uncertainty and inaccuracy in diagnosing prostate cancer: this means that at least 60% of cancers are missed; resulting in a 30%-40% re-biopsy rate. The gold standard for prostate biopsy (a 35-year-old pathway) is only accurately able to find up to 44% of prostate cancers within a cohort of men,” adds Boustead.
Therefore, he is one of the first urologists looking to invest in the Philips Invivo UroNav in South Africa in the future.
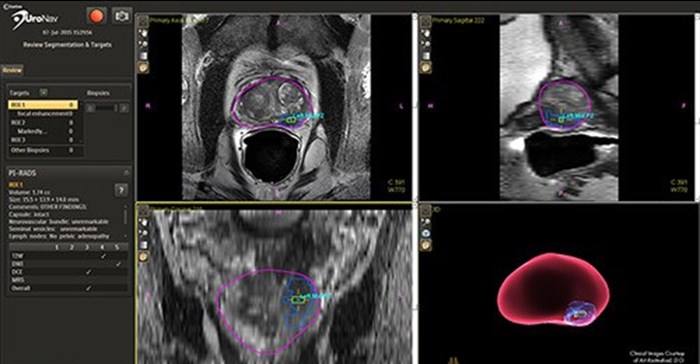
The system uses magnetic resonance (MR) imaging, fused with live ultrasound guidance in conjunction with electromagnetic tracking to plan, guide, and document prostate biopsies. It simultaneously displays registered MR and ultrasound images and the projected needle path relative to the suspicious target lesion during the biopsy procedure and guides the urologist in real-time. What this essentially means is that with this high resolution data and innovative targeting tools we can identify specific areas within the prostate gland that are suspicious and require further evaluation.
“This critical exchange of diagnostic information fosters enhanced collaboration between radiology and urology in the assessment and biopsy of suspicious prostate lesions,” says Boustead.
Performing a biopsy with MR/US fusion holds the potential to improve the sensitivity and specificity of prostate biopsies. This results in a reduced incidence rate of false negative biopsy results.