Study compares gastric bypass to conventional medical treatments and lifestyle modifications in mildly obese and non-obese patients.

(Image: Wikimedia Commons)
A new clinical trial at New York-Presbyterian Hospital/Weill Cornell Medical Centre is among the first to test surgery specifically for Type 2 diabetes. The aim of the study is to understand whether surgery can control diabetes, as well or even better than the best medical treatment available today. This is the first study of its kind open to patients who are overweight or mildly obese.
Under current guidelines, bariatric surgery is only indicated for the treatment of severe or morbid obesity, defined as having a body mass index (BMI) of 35 or greater. By contrast, the new study is open to patients with a BMI as low as 26. Normal-weight individuals have BMI ranging between 19 and 25 and overweight individuals have BMI between 26 and 29, whereas a BMI above 30 defines obesity. Patients with a BMI below 26 and above 35 will not be considered for enrolment in the trial.
The benefits of gastric bypass surgery
Previous research has shown that in severely obese patients (BMI greater than 35) gastric bypass surgery is a safe and effective way to treat Type 2 diabetes. It has been shown to improve or normalise blood glucose levels, reduce or even eliminate the need for medication, and lower the risk for diabetes-related death.
"There is preliminary evidence suggesting that that these results are attainable even in overweight or mildly-obese patients," says Dr. Francesco Rubino, chief of the gastrointestinal metabolic surgery program at New York-Presbyterian Hospital/Weill Cornell Medical Centre and associate professor of surgery at Weill Cornell Medical College.
In support of this belief, recommendations from the American Diabetes Association's January 2009 issue of Standards of Care: Diabetes Care, and from the Diabetes Surgery Summit Consensus Conference, published in the March 2010 issue Annals of Surgery, suggest that randomised clinical trials for the study of surgery in patients with BMI below 35 are priority for diabetes research.
Rigorous, comparative trials needed
"Having a potentially effective surgical option against diabetes does not mean that surgery is the best choice for every diabetic patient," Dr. Rubino adds. "We need rigorous, comparative clinical trials, like this one, in order to better understand when to prioritise surgery and when to recommend traditional medical treatment."
(Image: Wikimedia Commons)
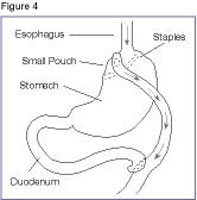
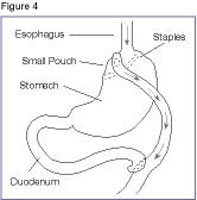
The new study is enrolling 50 patients with Type 2 diabetes who will be randomised to receive surgery - specifically, Roux-en-Y Gastric Bypass - or traditional medical therapy and intensive lifestyle modification. All patients will be counselled in lifestyle modification techniques like diet and exercise.
Dr. Rubino expects that there will be medical advantages for patients in both arms of the trial since those assigned to the medical arm will receive the most rigorous medical diabetes therapy available. A multidisciplinary team of diabetes and nutrition experts will take care of patients using the most current, approved drugs for diabetes as well as an intensive approach to lifestyle changes. Patients in the medical arm will also be offered the chance to switch study arms and have surgery free of charge after the study is complete, or earlier should their diabetes remain poorly controlled after medical and lifestyle therapy.
Beyond BMI
Dr. Rubino and his co-investigators believe their study may also help identify better criteria than BMI for selection of surgical candidates. "Using strictly BMI-based criteria may be practical, but it is medically inappropriate because, on its own. BMI does not accurately define the severity of diabetes or identify patients who are best suited to benefit from a surgical approach," says Dr. Rubino. "New criteria would not only help patients and clinicians, but also payers."
Because insurers use BMI-based criteria, bariatric surgery is currently not covered for patients with a BMI less than 35, regardless of the severity of their disease. Consequently, the study at New York-Presbyterian/Weill Cornell is supported by a research grant from Covidien covering the cost of surgery for patients enrolled in the study.
A Look at How Diabetes Surgery Works
Previous research by Dr. Rubino studied how bariatric surgery alleviates diabetes, showing that the effect on diabetes is not entirely explained by a person's weight loss. In fact, the gastrointestinal tract serves as an endocrine organ and a key player in the regulation of insulin secretion, body weight and appetite, which is why altering the GI tract has such profound metabolic effects.
The current study aims to shed more light on the mechanisms of action of gastric bypass on diabetes. To do this, Dr. Rubino and his co-investigators will measure gut hormone responses to meal stimulation when an equivalent amount of weight loss has been achieved in both surgically and conventionally treated patients. This design may help uncover endocrine effects specific to gastric bypass surgery beyond those associated with non-surgical weight loss. "Understanding how gastric bypass surgery functions may help us learn how diabetes works," Dr. Rubino says. "This knowledge has the potential to lead to the development of new minimally invasive procedures, devices interventions and better pharmaceutical treatments."
Toward an International Consortium
Dr. Rubino hopes that the current study will be a template for larger, international studies. "We intend this study to serve as a core protocol for similar randomised clinical trials independently run at other institutions as part of a worldwide consortium coordinated through the Diabetes Surgery Centre at New York-Presbyterian/Weill Cornell," he says. "The consortium will provide a larger pool of patients allowing researchers to better evaluate the impact of surgery on various health measures, including cardiovascular risk and life expectancy."
The global prevalence of Type 2 diabetes is rising dramatically. "If proven successful, diabetes surgery has the potential to help millions of patients in the US and worldwide," Dr Rubino says.
According to International Diabetes Federation (IDF), there are currently 285 million people with the disease around the world, a number that is expected to rise to 438 million by 2030. Diabetes is one of the greatest public health threats in the 21st century and a risk factor for vascular damage and eye, kidney and cardiovascular diseases, as well as death. Type 2 diabetes results from inadequate insulin production and action, and is associated with metabolic dysfunctions involving lipid metabolism and blood pressure regulation.
Source: New York- Presbyterian Hospital/Weill Cornell Medical Centre/Weill Cornell Medical College