
Top stories






More news


Marketing & Media
Ads are coming to AI. Does that really have to be such a bad thing?













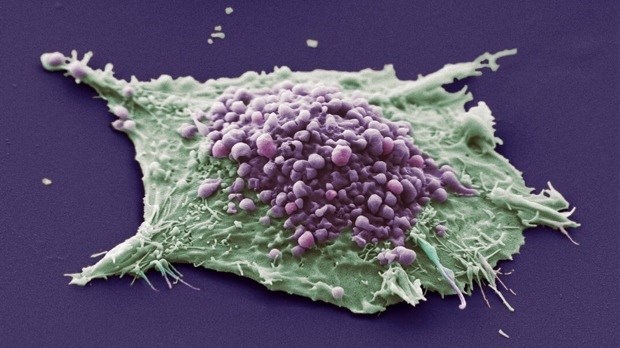
The findings suggest that the two types of small cell lung cancer could each be treated differently, according to the researchers from the Huntsman Cancer Institute (HCI) at the University of Utah in the US.
Lung cancers are usually defined as either small cell or non-small cell. But these latest results, published in the journal Cancer Cell, suggest there may be further differences among the small cell tumours.
Experts believe that the discovery could lead to new forms of treatment that target each specific tumour type.
“Survival for small cell lung cancer is low and how we treat the disease hasn’t really changed over the last 20 years. We urgently need new drugs for this hard to treat cancer,” said Dr Alastair Greystoke from the Cancer Research UK Newcastle Cancer Centre.
“The drugs used in this study have shown some promise in this disease. So these latest findings will help us work out how best to target them in small cell lung cancer.”
There are no genetic tests available for small cell lung cancer patients to select different treatments, so they are all treated in much the same way, says Professor Trudy Oliver, an investigator at HCI who led the study.
But the new research shows that, in mice, small cell tumours don’t all act alike. If further research shows the same results in humans, this could eventually change how some patients are treated.
The team created the first known replica of a small cell tumour subgroup called C-MYC in mice. This group, which is based on genetic differences, makes up around 1 in 5 patients with small cell lung cancer.
They found that C-MYC tumours look different to other tumours under the microscope and are very aggressive – growing and spreading faster. And they also responded differently to treatment.
The new research also found a drug that could be effective against these aggressive tumours.
The drug – called an Aurora kinase inhibitor – improved survival for mice when combined with chemotherapy.
While chemotherapy starts out effective in around 4 in 5 patients, the tumours can quickly develop resistance to the treatment.
“This important research gives us new information on how this type of lung cancer becomes resistant to chemotherapy so quickly.” Dr Greystoke added.
“Even more importantly, it tells us how we can target this problem.”
References
Mollaoglu, G. et al. (2017). MYC Drives Progression of Small Cell Lung Cancer to a Variant Neuroendocrine Subtype with Vulnerability to Aurora Kinase Inhibition. Cancer Cell. 31, 1–16. DOI: http://dx.doi.org/10.1016/j.ccell.2016.12.005
Source: Cancer Research UK