
Top stories






More news


Marketing & Media
Ads are coming to AI. Does that really have to be such a bad thing?













The study also identifies a potential remedy. A drug now in clinical trials for other indications reversed symptoms of chemo brain, as the condition is known, in a mouse model, the researchers found.
Chemo brain is becoming more common as cancer therapies increasingly allow patients to live many years beyond their diagnoses. There are 15.5-million cancer survivors alive today in the United States, a figure expected to reach 20-million by 2026, according to the National Cancer Institute. But the cognitive side effects of cancer treatment can be debilitating and prolonged: Adults may be unable to return to work, and children often struggle in school.
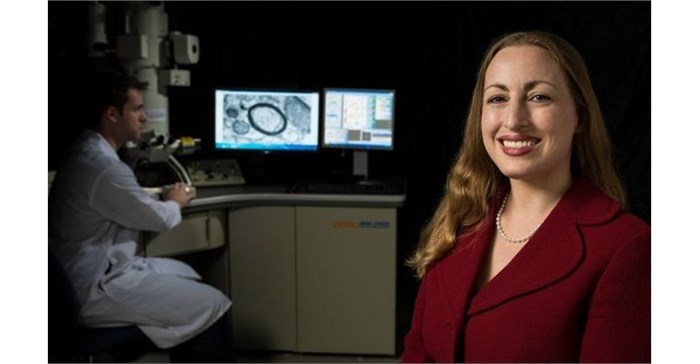
“Cognitive dysfunction after cancer therapy is a real and recognised syndrome,” said Dr Michelle Monje, associate professor of neurology and neurological sciences and the study’s senior author. “In addition to existing symptomatic therapies — which many patients don’t know about — we are now homing in on potential interventions to promote normalisation of the disorders induced by cancer drugs. There’s real hope that we can intervene, induce regeneration and prevent damage in the brain.”
Chemo brain is especially severe in childhood cancer patients, Monje added, and children have the most to gain from better remedies.
In addition to neurons, which transmit nerve impulses, the brain’s white matter contains other cells that help the neurons function. The research focused on three types of those cells: oligodendrocytes, which produce and maintain myelin, the fatty insulating sheath around nerve fibers; astrocytes, which link neurons to their blood supply, promote proper connections between neurons and maintain the neurons’ environment; and microglia, immune cells that can engulf and destroy foreign invaders in the brain, as well as sculpt neural circuitry.
Comparing postmortem frontal lobe brain tissue from children who had and had not received chemotherapy, the researchers showed that there were far fewer oligodendrocyte lineage cells in the brains of the chemotherapy-treated children.
To figure out what was happening to these cells, the researchers injected young mice with methotrexate at levels designed to replicate human exposures during cancer treatment. The mice received three doses at weekly intervals. Four weeks later, the researchers compared the mice’s brains to those of mice that had not received the drug.
Methotrexate chemotherapy was found to damage the brain’s populations of oligodendrocyte precursor cells. Normally, these cells can quickly divide to replace any that are lost, but after methotrexate was administered, this self-renewal process did not happen correctly. More precursor cells than normal were starting down the path of maturation to oligodendrocytes, but they were getting stuck in an intermediate, immature state. The same problem was seen in mice brains six months after methotrexate was administered.
Transmission electron microscopy of the mouse brains after methotrexate administration revealed deficiencies in the thickness of the myelin insulation around nerve fibres, similar to changes in the brains of humans who have received chemotherapy. Mice exposed to methotrexate also exhibited behavioural problems after four weeks that were similar to humans with chemo brain, including motor impairment (slower movement of their forepaws), signs of anxiety on an “open field” test used to assess how threatened the animal feels in an unsheltered environment, and impaired attention and short-term memory function, evidenced by the inability to discern between novel and familiar objects — a symptom that persisted for six months after methotrexate was given.
The researchers injected oligodendrocyte precursor cells from healthy animals into the brains of animals that had received methotrexate to see if the cells’ maturation problems were caused by some aspect of the brain environment after chemotherapy. The precursor cells still began maturing at higher-than-normal rates but did not get stuck partway through the maturation process, indicating that the brain environment was partly responsible for the cells’ abnormal maturation.
Further study showed that microglia, the brain’s immune cells, were persistently activated after methotrexate exposure for at least six months. The activated microglia caused problems for astrocytes, the cells that help neurons get nutrients and function properly. Administering a drug that selectively depleted microglia to mice that had been treated with methotrexate reversed many of the cognitive symptoms of chemo brain and reversed the abnormalities in maturation of oligodendrocyte precursor cells, activation of astrocytes and myelin thickness.
“The biology of this disease really underscores how important intercellular crosstalk is,” Monje said. “Every major neural cell type is affected in this pathophysiology.” She suspects this type of complex dysfunction may also underlie other cognitive disorders. “I think that is probably more the rule than the exception,” she said.
More research is needed to understand exactly how the different cell types are signalling to each other, as well as when and how medications could be best deployed against chemo brain.
“If we understand the cellular and molecular mechanisms that contribute to cognitive dysfunction after cancer therapy, that will help us develop strategies for effective treatment,” Monje said.