
Top stories






More news


Marketing & Media
Ads are coming to AI. Does that really have to be such a bad thing?













The standard treatment for older women with early stage breast cancer includes breast-conserving surgery, typically followed by radiation therapy to reduce the risk of breast cancer recurrence. Rather than irradiating larger areas of the breast, as in whole breast irradiation, brachytherapy temporarily implants radiation sources in catheters within the surgical site. This technique delivers larger and fewer radiation doses directly to the breast tissue, which results in a shortened treatment time and, proponents of the therapy believe, decreased toxicity to surrounding healthy tissue.
"This treatment method seems ideal in theory, but we found it concerning that such an important clinical decision that affects so many women was being made on the basis of theory, rather than scientific evidence," said the study's lead author Dr. Cary P. Gross, associate professor of internal medicine at Yale School of Medicine. "Despite the absence of large randomized controlled trials comparing these two treatments, brachytherapy has become increasingly popular, in part because of a theoretically lower rate of complications."
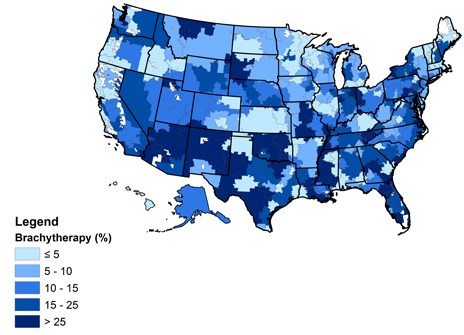
To test the theory, Gross' team studied a national sample of approximately 30,000 women with Medicare coverage and found that 15.8% of women undergoing radiation therapy received brachytherapy in 2008-2009, up from less than 1% in 2000 and 10% in 2006. There was substantial variation in brachytherapy use across the country, ranging from less than 5% of patients in some areas to over 70% in others.
The team found that the use of brachytherapy was associated with a 16.9% higher rate of wound and skin complications in the year after treatment compared to whole breast irradiation. There was no significant difference in the rate of deep tissue or bone complications between the two treatments.
"This study highlights the importance of conducting comparative effectiveness research before a new treatment becomes widespread," said Gross, who is co-director of the Robert Wood Johnson Clinical Scholars Program at Yale. "Medicare is spending significantly more money to cover this treatment, which potentially exposes women to a higher risk of complications than the 'tried and true' whole breast irradiation."
Other Yale authors on the study include Carolyn Presley, Pamela Soulos, Jeph Herrin, James Yu, Kenneth Roberts, and Jessica Long. Gross is the director of the Cancer Outcomes, Public Policy, and Effectiveness Research (COPPER) Center at the Yale Cancer Center.
The study was funded by a grant from the National Cancer Institute (RO1CA149045).
Source: Yale University