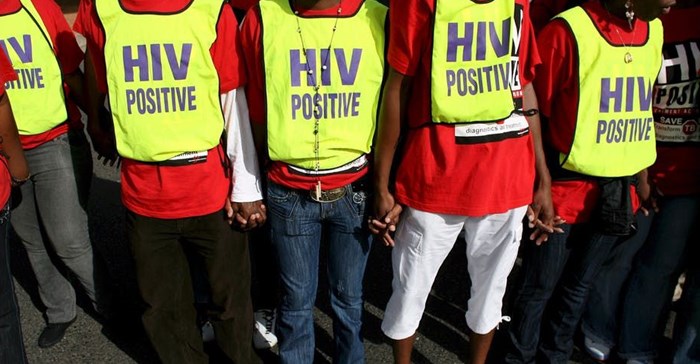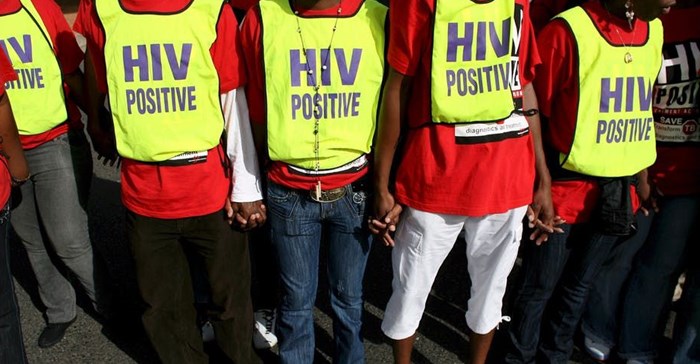
A number of factors contribute to the lower rates of uptake of HIV treatment by adolescents. Nic Bothma/EPA
Many countries have made substantial progress towards achieving these goals. But many have not. In particular, there are important groups of people at high risk, such as adolescents, whose progress is below the national average. These populations contribute the most to the ongoing transmission of HIV.
Adolescents – aged between 10 and 19 – especially female adolescents, continue to show high infection rates. Worldwide, 25% of all new infections are in adolescent girls and young women aged between 15 and 24. And unlike most age groups, adolescent mortality is increasing, with HIV being the leading cause of adolescent death in Africa.
Adolescents are also less likely to seek HIV services, or stay on treatment. HIV treatment outcomes, including retention, are worse for this age group than for adults.
This is true for South Africa too.
The country’s HIV treatment programme is expanding and the number of adolescents receiving care is growing. But our recent study shows that many adolescents who tested for HIV and had a blood test to measure the stage of HIV disease don’t start antiretroviral therapy.
This is a missed opportunity to engage adolescents already at a facility and link them to treatment successfully. By 2016, two thirds of young South Africans living with HIV were on antiretroviral therapy. This is encouraging but it’s still far off the UN’s 90% target.
Evidence from other work suggests that current models of HIV care aren’t meeting the unique needs of this group. This shows that South Africa’s health system needs to be adapted to deliver effective HIV care to adolescents.
What we found
We used routinely collected laboratory data from South Africa’s national HIV programme to estimate the total number of children and adolescents (aged 1-19 years) entering HIV care. The key finding was a 10-fold increase in the number of adolescents aged 15-19 years on antiretroviral therapy between 2013 and 2016 compared with 2005-2008.
Despite this growth there are still large gaps in successful linkage to treatment. Only 50% of those aged 15-19 successfully initiated antiretroviral therapy through to viral load testing. This is a test that measures the effectiveness of the treatment and usually takes place at six months, one year and then annually after treatment is started.
We didn’t look at long-term retention, so our research doesn’t speak to whether they are still on treatment now or even alive. We looked specifically at uptake of antiretroviral therapy after entering into HIV care.
This is an important finding because adolescence is a critical developmental transition stage from childhood to adulthood. We suggest that there are a number of factors that contribute to the lower rates of uptake of HIV treatment at this stage of life.
The first is that adolescents with HIV can be caught between paediatric and adult services that are unable to address their special needs. These include disclosure of HIV status, stigma, discrimination, sexual health and social support and other factors that impact their ability to move successfully through the HIV care cascade. This refers to the steps that people with HIV go through from diagnosis to viral suppression. It also shows the proportion of people accessing services at each stage of care.
Another factor affecting the rate of treatment among adolescents is that they are dealing with changes in parental versus personal responsibility for maintaining their health. They may be taking more risks, relying more on their peers for support and becoming more interested in serious sexual relationships. They may drop out from treatment to avoid disclosing their activities.
Research has shown that adolescents are at increased risk of infection and have lower rates of entry into care than adults. They also have higher rates of loss from care. But, until now, no national description of the stages in the adolescent HIV care cascade has been available to guide the way resources are targeted.
Our research provides this national perspective of the early stages of the care cascade. It gives a better idea of which young people are in need and when they are at risk of dropping out of care. It’s also important to track how they move from adolescent to adult care and how to keep them in care.
Next steps
Several factors will have an impact on the numbers of adolescents accessing HIV care in the coming years.
One is the success of programmes addressing prevention of mother-to-child transmission of HIV. Another is the extent to which adolescents get tested for HIV, how many go on treatment, and how many stay on it.
If these gaps were closed and antiretroviral treatment uptake increased to the 90% targets, the adolescent population on treatment in South Africa could nearly double in the next five years.
This expansion could have a powerful impact in breaking HIV transmission chains among adolescents. It also highlights why it’s important for the country’s health systems to understand and meet the needs of this group.
For example, traditional ways of getting care – having to go to a clinic or hospital to get tested and treated – don’t seem well-suited to the needs of many adolescents. They may be put off by the operating hours, poor relationships with staff, perceived stigma and loss of confidentiality.
South Africa is already trying to find more flexible ways to address some of these challenges. Adherence clubs – where HIV treatment and support is offered at times and locations convenient for specific groups of people – are one way of getting health care without having to visit a clinic. Mobile app-based technology could also offer awareness and education services that appeal to adolescents.
This article is republished from The Conversation under a Creative Commons license. Read the original article.