
Top stories





ESG & Sustainability#BudgetSpeech2026: SRD grant unchanged, other Sassa social grants see hike
18 hours

More news











ESG & Sustainability
South Africa’s carbon tax should stay: climate scientists explain why

















Moreover, the rate of vaccination against viral hepatitis in patients with chronic liver disease and type 2 diabetes is relatively low, and these patients are at increased risk of severe liver injury once infected. DDW is the largest international gathering of physicians and researchers in the field of gastroenterology, hepatology, endoscopy and gastrointestinal surgery.
"These studies suggest that innovative detection practices, as well as different methods of screening, can go a very long way in preventing liver-related diseases and can stave off premature death due to liver disease," said Adrian Di Bisceglie, MD, chairman, department of internal medicine, Saint Louis University.
Low vaccination rates against hepatitis A and hepatitis B in patients with chronic liver disease and with type 2 diabetes: a study of the US population (Abstract #Su1020)
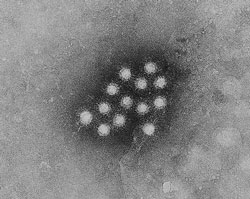
Both hepatitis A (HAV) and hepatitis B (HBV) may cause severe liver injury, which is often even worse in patients with underlying chronic liver disease (CLD). Vaccination rates against HAV and HBV are relatively low in patients with CLD and type 2 diabetes; however, these patients are at risk of severe liver injury if they become acutely infected. Therefore, mechanisms should be put in place to help increase vaccination rates for this high-risk population, according to new research from the Inova Fairfax Hospital.
Patients who suffer from chronic liver disease are already more prone to develop severe disease; when they are afflicted with additional liver trouble, the injury is exacerbated and they can suffer liver failure, resulting in the need for a liver transplant or, in even more severe cases, death. This is true not only of patients with CLD, but patients with type 2 diabetes are also at risk, since many people with diabetes have "undiagnosed" non-alcoholic fatty liver disease (NAFLD). For this reason, when type 2 diabetes patients suffer another acute injury, such as HBV, they can have a severe course, similar to those with CLD.
Because of the potential for injury, a number of professional societies have recommended some form of vaccination against HAV and HBV for patients with chronic liver disease in general, yet some studies to date show low rates of vaccination, despite these recommendations.
Investigators led by Zobair M. Younossi, MD, vice president of research for Inova Health System in Falls Church, VA, and executive director of the centre for liver diseases at Inova Fairfax Hospital, looked at the National Health and Nutrition Examination Survey, a population-based survey with a history of clinical and lab data, to identify trends in the rate of vaccinations against HAV and HBV in the general population. They looked at two cycles, which included 22 466 adults, 3239 of whom had CLD, and 2480 who had DM. HAV vaccination rates increased only in the NAFLD group, while HBV vaccination increased for HCV and NAFLD, but all increases were relative to rates of increase among the general population.
"What we found was that although the rate of vaccination for both hepatitis A and B is increasing in the general population and in patients with chronic liver disease and type 2 diabetes, the overall rate is quite low," said Dr. Younossi. At most, about 30% of patients with CLD were vaccinated. Researchers found that while there was an increase in the rate of HAV and HBV vaccinations between these two groups, in patients with CLD and type 2 diabetes, the rates remained very low.
Dr. Younossi said he expects the low rates are due to a number of factors. In part it may be that health-care providers do not have an appropriate understanding or appreciation of the importance of HAV and HBV vaccination in patients with CLD.
There may also be barriers to access of vaccines - for example, vaccines have to be given in multiple shots over time as a series, but primary care physicians or gastroenterology offices may not be equipped to administer and store vaccinations, presenting a challenge to access for many patients.
For these reasons, a different approach is needed that entails effective education programs taught to both primary care physicians, as well as specialists, to help educate them about the importance of providing vaccinations to their patients with CLD and DM. As part of this solution, providers might look at how drug stores, pharmacies, community health centres and other appropriate locations could help raise vaccination rates, in an effort to get them to more people more effectively. Dr. Younossi added that less expensive vaccines would also help, especially for uninsured or underinsured patients. "This is an important public health issue, and public health policymakers need to develop strategies to make better vaccination mechanisms available to individuals with chronic liver disease," he said.
Dr. Younossi presented these data on Sunday, 8 May 8 at DDW.
Screening individuals for hepatitis C virus (HCV) based on age rather than risk factors could have significant implications for the prevention of liver disease and premature death due to liver disease, according to new research led by Lisa McGarry, MPH, director of health economics and outcomes research at Innovus, part of Ingenix Life Sciences, in Medford, MA. Between three and four million Americans are infected with HCV, and more than two million are in what investigators call the baby boomer plus birth cohort (individuals born between 1945 and 1970).
Investigators sought to study this population because current risk-based screening practices have had limited success; current estimates suggest that less than 3% of infected individuals are screened each year. Research in recent years has identified high HCV incidence in baby boomers, most of who do not know they were infected, mainly because they were probably infected years earlier and would not currently be considered high risk. Under current practices, someone without symptoms of liver disease who is not an intravenous drug user would not be perceived as high risk and thus, would probably not be screened.
Further compounding the problem, HCV can lie dormant for many years. People may not show symptoms until 20 years or longer after they have been infected, said McGarry.
Researchers used an epidemiologically based mathematical model to project economic and clinical outcomes of a birth-cohort screening program. The first part of the model sought to determine how many people would currently be infected and undiagnosed, and how far the disease would have progressed in this population. Then, they looked at implementing a screening program targeted at the baby boomer plus birth cohort versus current low levels of risk-based screening. Finally, they ran the model forward to the remainder of people's lifetime to see how screening would affect progression to advanced liver disease (AdvLD) and mortality.
The model suggests the following:
McGarry added that there are several HCV treatments in development, which would further increase the benefit of screening. "This study shows that targeted screening based on age rather than risk factors would lead to more identification of HCV-infected individuals and thus, more treatment and prevention of advanced liver disease. Screening is potentially a smart investment, comparable to widely accepted preventive health practices. In particular, screening for HCV now may reduce future costs to Medicare."
Funding for the study was provided in part by Vertex Pharmaceuticals.
McGarry will present these data on Sunday, May 8 at 2:15 p.m. CT in S106B, McCormick Place.
Treating hepatitis C with a drug regimen that adds the protease inhibitor telaprevir to the standard therapy of pegylated interferon alfa-2a and ribavirin is effective, both for patients who have not responded to usual therapy and those who relapsed after treatment, according to researchers at the Scripps Clinic.
The findings in the international randomised, double-blind trial offer new hope to individuals with chronic hepatitis C, said Paul J. Pockros, MD, clinical director of research at the Scripps Translational Science Institute and head of the Scripps Clinic division of gastroenterology/hepatology.
"We saw excellent rates of sustained virologic response with telaprevir-based therapy," Dr. Pockros said. "There were dramatic improvements in all groups of patients, although the three-drug combination worked best for patients who had relapsed or only partially responded to standard therapy."
The study involved 662 patients with hepatitis C genotype 1, which is particularly difficult to treat. 70% of participants were male and 93% were Caucasian; about one out of four had cirrhosis.
Researchers evaluated the effectiveness, safety and tolerability of the telaprevir-based regimen, and their results confirmed those of previous trials. They also assessed whether the triple combination was more effective if it followed four weeks of standard therapy as a "lead-in strategy." They found no additional benefit to starting all three drugs simultaneously, Dr. Pockros said.
Funding for the multi-centre study was provided by Vertex Pharmaceuticals, which has developed telaprevir in collaboration with two overseas companies.
Dr. Pockros presented these data on Monday, 9 May 9 at DDW.
Digestive Disease Week 2011 (DDW) is reputed to be the largest international gathering of physicians, researchers and academics in the fields of gastroenterology, hepatology, endoscopy and gastrointestinal surgery. Jointly sponsored by the American Association for the Study of Liver Diseases, the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy and the Society for Surgery of the Alimentary Tract, DDW took place 7-10 May 2011 in Chicago. The meeting showcased more than 5000 abstracts and hundreds of lectures on the latest advances in GI research, medicine and technology.
Source: DDW 2011