
Top stories


ESG & Sustainability6 women using STEM to make the South African circular bioeconomy a reality
2 hours




More news























Construction & Engineering
Egypt plans $1bn Red Sea marina, hotel development



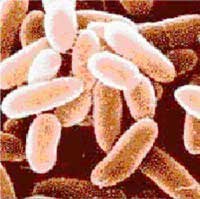
Anthrax is caused by Bacillus anthracis, a bacterium that forms seed-like structures called spores capable of reproducing the organism despite tremendous punishment. In recent years, anthrax has become a top choice as a biological warfare agent, according to the U.S. Department of Defence (DOD), because its spores can easily become airborne. It can be spread by mailed packages, missiles or crop-dusting planes. It can travel downwind for hundreds of miles and stay lodged in soil for decades. Following the Sept. 11, 2001, attacks, terrorists mailed letters coated with anthrax spores to 22 U.S. men and women, five of whom died. Saddam Hussein developed anthrax spore-filled weapons, and Boris Yeltsin said the former Soviet Union had a biological weapons program that dwarfed that of pre-war Iraq.
The U.S. military requires personnel in high-risk areas to be vaccinated with the only FDA-licensed human anthrax vaccine, BioThraxTM, produced by BioPort Corporation/Emergent Defence Operations. It was approved by the U.S. Food and Drug Administration in 1998, and about 1.8 million U.S. personnel have been vaccinated since then, according the Department of Defence. Those vaccinated are intended to receive a series of six shots, and then an annual booster shot. While 1.8 million have been vaccinated since 1998, just seven million doses have been handed out.
“Our study found that a mucosal delivery system promises to add a second layer of immune protection against anthrax by priming the disease-fighting cells in mucous membranes lining the nose along with those in the blood, and with just three doses,” said Mingtao Zeng, Ph.D. He is assistant professor within Department of Microbiology and Immunology at the University of Rochester Medical Center, and a study author along with Qingfu Xu, also at the medical center. “That, along with the addition of newly precision-designed vaccine components, should represent important steps in the race to provide troops with stronger protection in a vaccine that is easier to use.”
The study was in mice, but much of the evidence behind the currently approved vaccine was collected in animals as well. In a challenge common to many lines of vaccine research, it is “obviously unethical to test anthrax vaccines in humans using the real pathogen.”
In arguing for the value of the currently available vaccine, the military cites a CDC study from the 1950s where an older version of the current vaccine protected mill workers when both “skin” (cutaneous) and “lung” (inhalation) anthrax infections outbreak at their workplace. In the study, 25 out of 754 unvaccinated workers were infected with skin anthrax, while just one of 379 vaccinated workers was infected. During that study, five of the unvaccinated workers unexpectedly developed inhalation anthrax as well, and four of them died. None of the vaccinated workers developed inhalation anthrax. The same vaccine also protected 95% of monkeys and 97% of rabbits in other studies. The U.S. Food and Drug Administration has certified, and re-certified, that the current vaccine is safe and effective.
Despite these proofs, some critics argue that there has never been a large-scale study of the currently approved vaccine in humans, raising questions about how well the current vaccine would protect against a modern-day, weaponised version of anthrax. A few former soldiers are involved in lawsuits with the military because they refused to be injected with the vaccine, which they did not believe to be safe. The current vaccine was formulated before the revolution in molecular biology in the 1980s. Today, vaccines are designed “rationally,” based on precise understanding of molecular pathogenesis and protein structures. Older vaccines contained a mix of ingredients that were not always precisely defined.
Given these questions, vaccine designers worldwide have been seeking to design a vaccine made up of a more precise combination of the Bacillus anthracis antigens. In the latest attempt, the current study sought to improve on the current vaccine in two ways: deliver it mucosally and fine-tune its ingredients. Membranes lining the mouth, nose, and throat secrete mucus, a thick coating that protects these surfaces as they interact with the outside world. Mucosal membrane has its own set of disease-fighting cells concentrated in mucosa-associated lymphoid tissue (MALT) that are related to, but separate from, the immune cells operating in the bloodstream, lymph nodes and spleen.
Researchers believe a vaccine administered via the mucosal surface might prime both sets of immune cells, providing two layers of protection, and a very strong effect in the membranes that would be directly exposed to airborne anthrax spores. Vaccines injected by needle may prime only the systemic immune system. In addition, mucosal vaccination is painless, making it convenient for vaccine administration even when multiple doses are required, researchers said.
The purpose of the human immune system is to recognize and destroy invading organisms, and to remember and fight against them should they invade again. Without causing an actual infection, vaccines introduce weakened or detoxified versions of disease-related molecules to the system, which remembers them for next time. Once researchers confirm the kind of immune response needed to achieve protection, they can choose for inclusion in a multi-component vaccine the key antigens that trigger the strongest immune response. The immune system reacts, not to the presence of a whole bacterium or virus, but instead to specific proteins (antigens) on the surface of, or secreted by, the pathogen that reveal its identity.
Past studies have shown that anthrax kills by secreting three toxic proteins that cause the breakdown of key immune cells, and ultimately, the death of cells and tissues. Paradoxically, those same toxins, if changed slightly, may represent the best vaccine building blocks. The toxins are protective antigen (PA), lethal factor (LF), and oedema factor (EF). PA binds to receptors on the outer surface of immune cells called macrophages and forms a pore through which LF and EF can enter the cells. Once inside, LF signals for the cell to self-destruct, and EF causes a damaging inrush of fluid (e.g. inflammation). Since macrophages remove toxins from the body, their death causes a quick build-up of toxins fatal to cells.
Because PA plays such a central role in anthrax infection, human immune systems have evolved to recognize it well. However, it cannot cause disease itself until combined with LF or EF, and thus, makes the perfect vaccine ingredient. The current vaccine consists primarily of PA, with some undefined quantities of LF and EF, injected into the bloodstream. The re-designed study vaccine too has the biologically active portion of PA, PA63, as its first building block.
In the study's key innovation, Zeng's team next added a detoxified version of LF to PA63 to create an even stronger immune response. Past research has shown researchers can eliminate LF's toxicity by using molecular biology techniques to substitute out one of its amino acid building blocks. Detoxified mutant LF (mLF) was first assembled more than a decade ago in the lab of Stephen H. Leppla, Ph.D., acting lab chief at the Laboratory of Bacterial Diseases within the National institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health. Although first assembled a decade ago, no one had yet looked at whether it would make a good component for a candidate anthrax vaccine. The hope was that detoxified mLF could be safely administered into a host, and that the host's immune system would still recognize the detoxified version.
For the experiments, the team divided thirty-two mice into four groups of eight. Each group received a nasal spray three times over four weeks that contained either PA alone, detoxified mLF alone, a combination of PA and mLF at the same doses or an inactive control solution. The animals were then subcutaneously challenged with B. anthracis Sterne spores.
In a dramatic result, all mice vaccinated with the combination vaccine (60 µg PA63/30 µg mLF) were protected against anthrax spore exposure and survived. Just 60% of those vaccinated with only PA63 survived, and just 30% of those receiving mLF alone. All control animals inoculated with saline died within 5 days of spore challenge.
Reflecting the survival results, intranasal vaccination with the combination PA63/mLF elicited significantly higher antibody responses against PA or LF than vaccination with the same amount of individual PA63 or mLF at all time points measured (P values < 0.05). The data suggested that PA63 and mLF have a mutual enhancement effect, researchers said, in terms of evoking an immune response. Two types of immune system cells, T cells and antibodies, enable the system to “remember” bacterial incursions, and levels of each were followed closely.
To see if intranasal mucosal vaccination with the combination vaccine elicited mucosal immune protection, the team measured anti-PA and anti-LF antibody levels in saliva, nasal wash, and other mucosal samples from vaccinated animals. Three doses of 60 µg of PA63/30 µg mLF resulted in considerably higher levels of mucosal anti-PA and anti-LF antibody responses than vaccination with either PA63 or mLF alone.
In addition, modern, protein-based vaccine work like the current study uses for experiments only specific and detoxified proteins that resemble those created by the bacteria, not the whole, anthrax-causing organism, making it much safer to work with. Should the new combination be approved for use in humans in the future, it would be much easier, safer and less expensive to manufacture for the same reason, researchers said.
“This study was the first to demonstrate that the detoxified anthrax lethal toxin could be used as an effective mucosal anthrax vaccine without any adjuvant,” Zeng said. “Other antigens such as N-terminal fragment of oedema factor, spore-associated glycoprotein, capsular poly-gamma-d-glutamic acid and various pieces of B. anthracis have also shown promise as candidate vaccine components, and a future vaccine may contain some of them along with the ones we tested here.”