Malawi races towards global HIV targets
90-90-90 strategy
This should be bad news for Malawi, which was recently credited for adopting and implementing progressive HIV policies in the roll out the World Health Organisation (WHO)-recommended public health approach to HIV prevention, detailed in Malawi’s 2011-2016 National HIV and Aids Strategic Plan.
The United Nations Programme on HIV and Aids (UNAids) 90:90:90 targets seek countries’ commitment to ensure that 90% of people living with HIV and Aids (PLHIV) should know their status by 2020, 90% of people diagnosed of HIV to be on ART by 2020 and 90% of patients on ART to be retained in care and have their viral load suppressed by 2020.
These targets have set the frame for the new Malawi National Strategic Plan (NSP) for HIV response 2015-2020 and concretely mean the aim is for 81% of people living with HIV (PLHIV) to be initiated and sustained on treatment and 73% of all PLHIV to be virologically suppressed.
Through this plan, it is predicted that adult HIV incidence will decrease to 0.2 (17,000 new infections per year) and paediatric infections to decrease to 3,900 per year.
To achieve these targets, high impact interventions must be identified at each step of the cascade.
Areas of disconnect
Various HIV and Aids experts do admit that there are still areas of disconnect in the implementation of these policies, which are likely to contribute to across the HIV diagnosis, care, and treatment continuum.
For example, there is a lack of clear guidelines on how laypeople can be involved in linking people to care and treatment.
The policy on home visits for clients who miss appointments is also unclear, reducing opportunities to return clients to care. In light of the ambitious 90:90:90 targets, these gaps in policy-to-practice sometimes necessitate implementation approaches, which extend beyond what is written in policy guidance.
Khonyongwa says assisted by Malawi’s progressive policies on HIV/Aids, it appears possible that Malawi could attain these targets if authorities can employ innovative programme approaches to service delivery which help fill policy gaps.
“We just need to come up with strategies that can help us stop new infections. That way, we will be able to eliminate the virus by the set period,” he explains.
However, to achieve these goals, the community and health system must act together as one with the patient placed firmly at the centre of any strategy.
Community-based strategies
In Malawi, community leaders have been engaged in HIV programming to fight against stigma and discrimination, and to encourage care and support of HIV infected individuals, orphans and vulnerable children (OVCs) and the elderly; mobilising communities to access HIV prevention; promoting PMTCT and male involvement in PMTCT; and demanding accountability from HIV service providers.
Thus, Khonyongwa stresses that strengthening community-based strategies across the HIV prevention care and treatment cascade is vital to maintaining what has already been achieved and will prove more essential to reach the ambitious targets set for 2020.
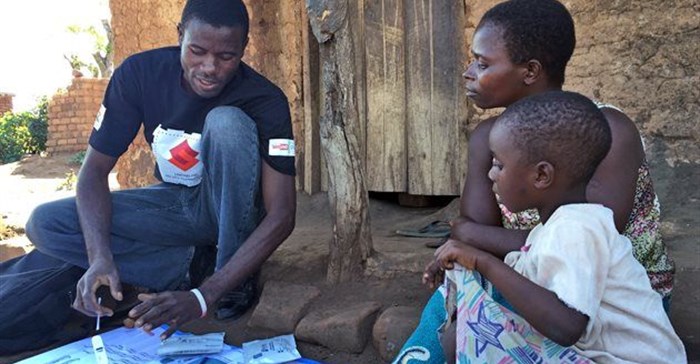
“And that is why with funding from the Global Fund is funding the project through Action Aid Malawi, MANET+ is training community volunteers and expert clients whom it is using to address psychosocial support and patient education, provide individual patient case management (appointment and defaulter tracing systems) and services that place the patient firmly at the centre of ART delivery,” he explains.
The major goal of the project is to maximise Malawi’s potential to achieve the three 90s targets by enhancing retention and ART adherence through use and engagement of community volunteers and expert clients (known HIV patients).
The project has also facilitated the introduction of adherence clubs, community ART groups (CAGs) and community ART distribution points in some districts such as Zomba.
While Malawi policy guidance (2011) does not specifically mention home visits, it describes group or individual counseling for clients with poor adherence and gives suggestions for improving adherence to treatment.
“For Malawi, the policy implications mean building on the foundation of progressive HIV policy by solidifying the cadre of dedicated HIV testers, strengthening human resources for health, and adding policy statements to incorporate peer volunteers for HIV support services,” Khonyongwa says.
Expert clients
Annie Likagwa, an HIV and Aids training facilitator at Chinansi Foundation in Balaka, says the use of expert clients for tracing clients loss-to-follow-up (LTFU) appeared to be effective, re-engaging in care people who would have otherwise remained lost.
Likagwa further states that expert clients are useful in pushing for and improving adherence to ART among patients, outreach and follow up, and other aspects of HIV-related care combined with phone reminders.
“In many of the examples, the critical work of lay counsellors, expert patients and community health workers underpin the intervention. These cadres support an activity at the facility but because they are community members, provide the essential link to the community to support tracing and home based interventions. Specific interventions for PMTCT [prevention of mother to child transmission] such as providing a mother mentor,” she says.
The UNAids deputy director for Regional Support Team for Eastern and Southern Africa, Dr Pierre Somse, recently hailed Malawi for the ‘high agreement between national and WHO policies for HIV testing and retention in care’.
Somse hinted that Malawi could also stand a chance of becoming a leader if government hastened the development of an overarching policy on community-oriented service delivery models that offers direction to implementers.














