Covid-19: Key trends impacting primary healthcare
Because primary healthcare is an important service and indicator for the overall management of patients, we looked at our data to help understand the impact on GP businesses and find ways to minimise the patient and financial implications.
Trend 1: Despite growth of Covid-19 cases, the average private GP experienced a major drop in patient consultations

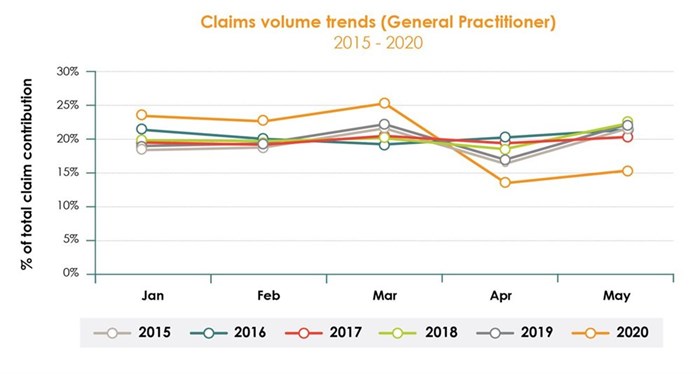
The graph shows a significant decrease in patient volumes for April and May. In fact, claims dropped by 50% in April in comparison to March. Although the number of GP visits are subject to a seasonal drop in April due to holidays, when we compare patient volumes from previous years (as depicted in the graph below), we can see that the drop in 2020 was much more severe.
Why is this important?
While a drop in GP visits could be attributed to lockdown restrictions, a significant drop that we’ve seen points to a much more worrying trend – the impact of treatment of chronic patients
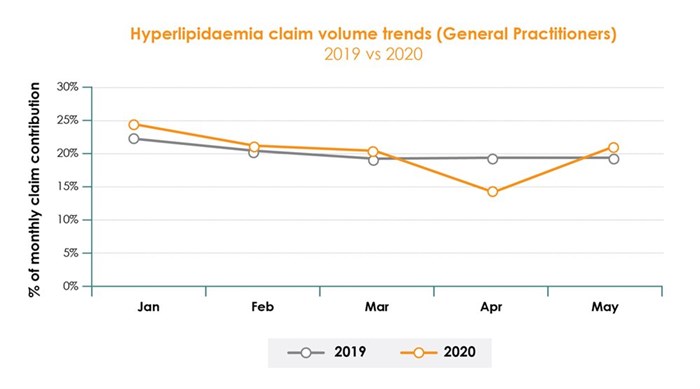
Looking at two prevalent chronic diseases in South Africa – Diabetes and Hyperlipidaemia – we can see an indicative drop in claim volumes during April. It is important to note that this data is representative of private healthcare only, and based on reports1 of missed appointments by HIV patients, diabetics and other patients needing chronic medication, the impact felt by the public sector was far more severe.
It can be surmised that patients were potentially avoiding healthcare practices for fear of contracting Covid-19. As a result, follow up appointments were missed, prescriptions were not filled, and regular check-ups were skipped. This doesn’t only pose a threat to patients in the short term, but it also poses a threat to the future healthcare burden, post Covid-19. By extension, the downtrend had an immediate financial impact on GP practices. Most practices will have experienced a drop in revenue that is significant enough to impact turnover for the entire financial year and making it difficult to cover costs.
There is also the potential long-term impact on the primary healthcare sector market that must be considered. For instance, the financial losses could result in practices closing their doors, GPs taking early retirement or a spike in immigration in the coming months. This, when GPs are already in demand, could result in a decrease in the number of GPs available to provide primary care services and poses an even bigger threat to the population health as the healthcare burden grows on a dwindling number of doctors.
Trend 2: General Practitioners had an increase in virtual consultations
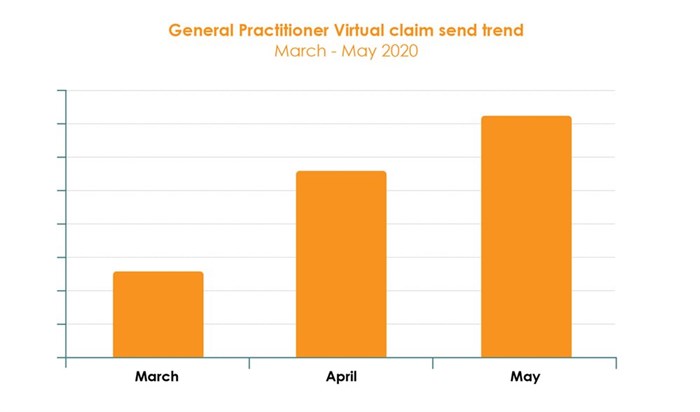
In the midst of the crisis, telehealth consultations became a safe, feasible way to see patients. The graph above indicates that while the adoption of telehealth is apparent, virtual consults only made up around 1% of total consults. While it’s true that Covid-19 took everyone by surprise, many practices were either slow to react or had too many technology restrictions to pivot their services to offer virtual appointments. Not only did those practices lose thousands of Rands in revenue, but patients also sought out alternative healthcare providers.
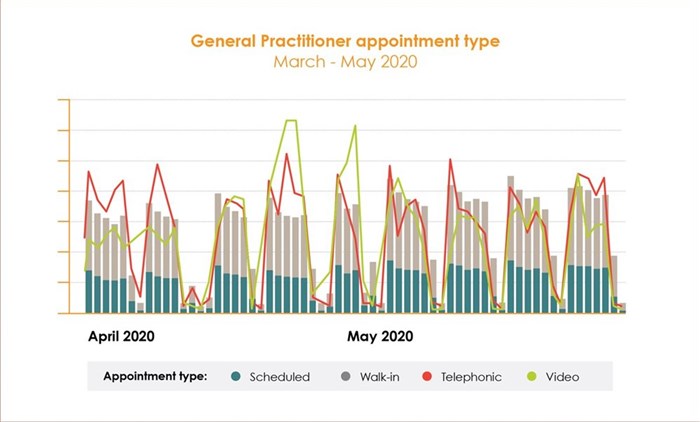
The data above demonstrates the uptake in adoption for both video and telephonic consults during the pandemic. We can also see that as the pandemic eased into level 4, video consults dropped but telephonic consults remained steady in usage.
Another observation we can make from our sales data is that there was an increase in demand for cloud-based practice management solutions. Doctors were faced with the same shift as the general population to adopt a more digital way of life. As a result, the need to manage medical practices from anywhere, at any time became more urgent as patients sought alternatives to in-person consults and doctors had to find ways to keep their staff and patients safe.
Why is this important?
1. The ability to consult digitally is not only a new norm, but an expectation for the future.
- Future novel diseases will continue to emerge, and practices need to be prepared. What Covid-19 has shown us is that medical practices need to future-proof against the same kind of economic hardship and be able to meet patient needs as they change.
- The population at large has been forced to adopt more digital tools to carry out their day-to-day activities. As people become more accustomed to using technology to live their lives, their expectations will rapidly extend to include virtual consults as the norm.
- The trend is even more obvious when we look to our overseas counterparts. For example, in 2018, 18% of American doctors reported treating a patient via telehealth. During the pandemic, almost half (48%) of all US physicians said they had treated patients virtually, according to a recent survey2.
2. GPs are also seeing that there are certain consultation types that are better suited to video and others by telephonic means. This not only improves time efficiencies for the practice but also:
- It is markedly more convenient for particular patient populations, such as the elderly, patients with chronic diseases, patients who are busy and those who live or work far away from the practice
- it’s also far more suitable for specific consultations such as communicating test results or issuing repeat prescriptions
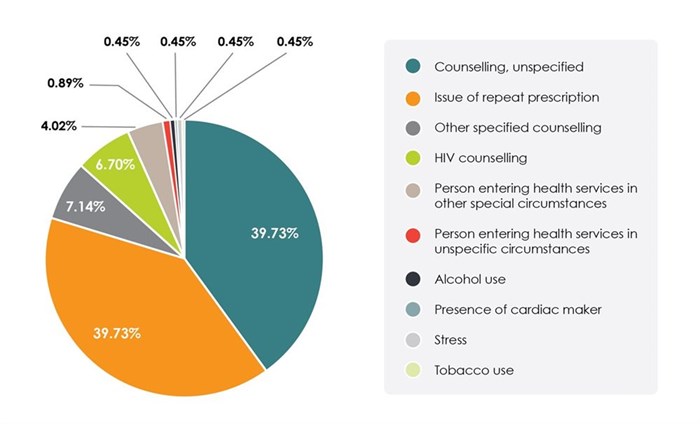
Trend 3: Counselling-related treatment was the top diagnosis for virtual consults
From the graph below, we can see the immediate impact that lockdown had on patients. The spike in mental health consults, counselling and substance use all lend themselves to being carried out virtually. It’s also a good indicator of what to expect from your patient population in the event of another outbreak or future pandemics.
Conclusion
If Covid-19 taught us anything, it’s that medical practices need to be prepared and agile enough to respond to what is affecting their patients, and the population as a whole. Practices that did not have the technological infrastructure took the hardest knock and while some took the opportunity to implement technology, it was unnecessarily stressful to roll out in the midst of so many changes.
If we rewind back to mid-March knowing what we know now, would your practice have suffered the same financial impact? And would you have opted to be more prepared? If nothing else, the crisis has cemented the fact that we need to be able to run businesses digitally. The world has effectively changed forever and being able to live and work remotely is no longer a nice to have, but a necessity.
Healthbridge has been helping doctors run their businesses for over 20 years. As technology leader in clinical healthcare solutions, click here to find out more about how you can future-proof your medical practice for good.
References
1. Evans, A., 2020. EXCLUSIVE | Unscientific And Nonsensical: Top Scientist Slams Government’S Lockdown Strategy | News24. [online] News24. Available at:
2. CB Insights Research. 2020. 24 Industries & Technologies That Will Shape The Post-Virus World – CB Insights Research. [online] Available at:
Healthbridge
Healthbridge is an innovative healthcare technology company that has been helping doctors run better businesses for 20 years. Healthbridge has pioneered a powerful range of products and services that help doctors to significantly improve the day-to-day running of their practices. This saves them more than R1bn a year in operational efficiencies. Healthbridge has over 5,000 medical practitioners on their books countrywide, including GP’s, Dentists, Optometrists, Specialists and Allied Healthcrare Professionals. Through their sophisticated medical information-exchange services, Healthbridge has integrated with hospitals, pathology laboratories, radiologists and medical aids. Healthbridge processes more than R30bn of transactions in real-time every year.
- Your security matters: IFX Brokers fraud awareness statement05 Sep 13:25
- Temperature control expertise: Mortuary fridges engineered for optimal preservation05 Aug 16:45
- Shattering stigma: Why drug rehabilitation centres are essential tools for a healthier society04 Jul 15:42
- Beyond traditional investments: Exploring the appeal of HFM for South African investors23 Apr 15:31
- Market insights: AvaTrade's impact on global trading trends09 Apr 08:40